Nova studija pokazuje drugi slučaj uspješne remisije HIV-a nakon transplantacije koštane srži
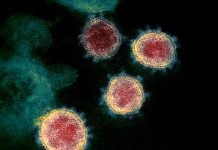
Najmanje milijun ljudi svake godine umre od uzroka povezanih s HIV-om, a gotovo 35 milijuna živi s njima HIV. HIV-1 (Virus humane imunodeficijencije) odgovoran je za većinu HIV infekcija diljem svijeta i prenosi se izravnim kontaktom s tjelesnim tekućinama zaraženim HIV-om. Virus napada i ubija ključne stanice našeg imunološkog sustava koje se bore protiv infekcija. Ne postoji lijek za HIV. Trenutno se HIV može liječiti samo lijekovima koji imaju sposobnost suzbijanja HIV-a virus. These drugs have to be taken life long and it is challenging plus a cost burden on the health system especially in low-and-middle-income countries. Only 59 percent of patients of HIV worldwide are receiving Antiretroviral therapy (ARV) and HIV virus is fast becoming resistant from many known drugs which itself is a major concern.
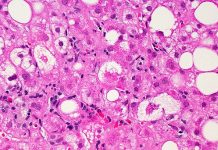
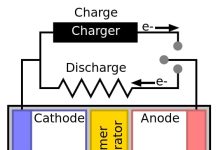
Transplantacija koštane srži (BMT) is a treatment used for leukemia, myeloma, lymphoma etc. Bone marrow, the soft tissue inside bones, makes blood-forming cells including the infection fighting white blood cells. A bone marrow transplant replaces unhealthy marrow with a healthy one. In the first case of successful HIV remission, an HIV-infected individual called ‘Berlin Patient’ who later revealed his name received a bone marrow transplant a decade ago when he was targeted to treat acute leukemia. He received two transplants along with total body irradiation which led to long-term HIV remisija.
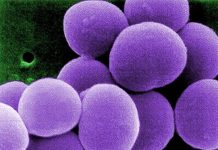
U novoj studiji objavljenoj u Priroda led by UCL and Imperial College London, the only second person has been shown to experience sustained remission from HIV-1 after a bone marrow transplant and stoppage of treatment. The anonymous adult male patient from UK was diagnosed with HIV infection in 2003 and was on antiretroviral therapy treatment since 2012. He was subsequently diagnosed with Hodgkin’s Lymphoma in the same year and he underwent chemotherapy. In 2016, he was given stem cell transplant from a donor who carried a genetic mutation which prevents expression of a most commonly used HIV receptor protein called CCR5. Such a donor is resistant to HIV-1 strain of the virus which specifically uses CCR5 receptor and thus the virus now cannot enter host cells. Since chemotherapy kills cells which are dividing, HIV could be targeted. From this understanding if one’s immune cells are replaced by cells which do not have CCR5 receptor, HIV can be prevented from rebounding after the treatment.
Transplantacija je provedena s manjim nuspojavama poput blage komplikacije uobičajene u transplantacijama u kojima imunološke stanice primatelja napadaju imunološke stanice donatora. Antiretrovirusno liječenje nastavljeno je 16 mjeseci nakon transplantacije prije donošenja odluke o prekidu liječenja kako bi se procijenila remisija HIV-1. Nakon ovoga, virusno opterećenje pacijenta i dalje je ostalo neotkriveno. Pacijent je ostao u remisiji nakon 18 mjeseci nakon što je prekinuta antiretrovirusna terapija jer imunološke stanice pacijenta nisu mogle proizvesti ključni CCR5 receptor. To ukupno trajanje je 35 mjeseci nakon transplantacije.
This is a second case of a patient exhibiting sustained remission of HIV-1 following a bone marrow transplant. One important difference in this second patient being that ‘Berlin Patient’ had received two transplants along with total body irradiation while this UK patient received only a single transplant and underwent less aggressive and lesser toxic approach of chemotherapy. Mild complications of similar nature were seen in both patients i.e. graft versus host disease. Achieving success in two different patients points towards developing strategies based on preventing CCR5 expression which might even cure HIV.
Authors state that they are monitoring the patient’s condition and cannot say with affirmation yet if he has been cured of HIV. This may not be a generalized appropriate treatment for HIV because of adverse effects and toxicity of chemotherapy. Also, bone-marrow transplants are expensive and carry risks. Nevertheless, it is a better approach with reduced intensity conditioning and no irradiation. Research could also focus on knocking out the CCR5 receptor using gene therapy in people with HIV.
***
{Izvorni istraživački rad možete pročitati klikom na vezu DOI koja se nalazi u nastavku na popisu citiranih izvora}
Izvor (i)
1. Gupta RK i sur. 2019. Remisija HIV-1 nakon transplantacije hematopoetskih matičnih stanica CCR5Δ32/Δ32. Priroda. http://dx.doi.org/10.1038/s41586-019-1027-4
2. Hütter G. i sur. 2009. Dugotrajna kontrola HIV-a transplantacijom CCR5 Delta32/Delta32 matičnih stanica. N Engl J Med. 360. https://doi.org/10.1056/NEJMoa0802905
3. Brown TR 2015. I Am the Berlin Patient: A Personal Reflection, Istraživanje AIDS-a i ljudski retrovirusi. 31(1). https://doi.org/10.1089/aid.2014.0224